The McNicholas Knee Clinic’s understanding and experience covers a vast range of orthopaedic procedures, from arthroscopic ‘key-hole’ surgery to ligament reconstruction, cartilage repair, partial, total and revision knee replacement.
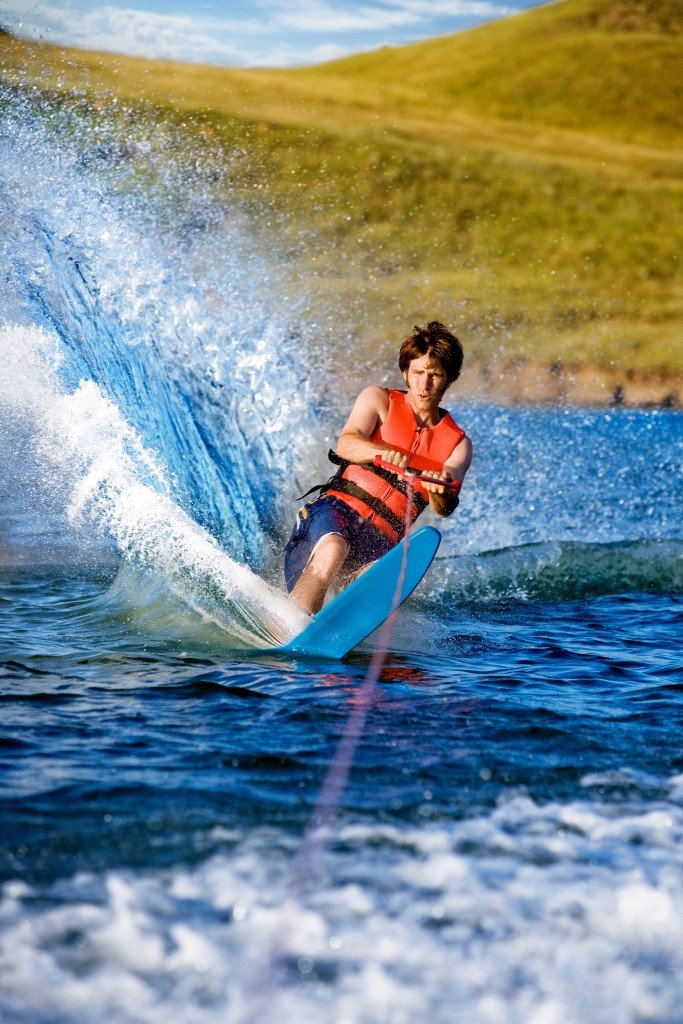
Sports injuries
They can get torn whilst playing sports, usually a twisting type injury often with immediate swelling of the knee.
After the initial injury, you may experience symptoms of pain, stiffness, locking and giving way of your knee.
The diagnosis is usually made following a detailed consultation including an examination of your knee. An X-ray may be taken as well as an MRI scan to diagnose the tear in your meniscus.
Treatment depends on the type of tear and how much trouble you are experiencing. If surgery is required it can involve trimming/removal of the meniscus or repairing the torn meniscus.
Further detailed information on meniscal surgery, complications and the rehabilitation process can be found in this patient information booklet:
Patient Information and Rehabilitation Guidelines Following Meniscal Surgery.pdf
The ACL is most likely to be injured in a non-contact twisting movement. A tearing or popping sensation is frequently reported at the time of injury and immediate swelling is common.
Symptoms include knee instability. The diagnosis is made via a thorough consultation including an examination of your knee. An X-ray and/or an MRI may be required. Treatment options include physiotherapy or surgical repair.
Further detailed information on ACL reconstruction, complications and the rehabilitation process can be found in this patient information booklet
Patient Information and Rehabilitation Guidelines following ACL reconstruction.pdf
You can also damage other ligaments of your knee at the same time, the postero-lateral corner (PLC). The PLC is made up of multiple ligaments which act to stabilise the knee and prevent excessive rotation. The PLC may also require repair.
Further detailed information on surgery involving ACL reconstruction with PLC reconstruction, complications and the rehabilitation process can be found in this patient information booklet:
Patient Information and Rehabilitation Guidelines following ACL and PLC reconstruction. pdf
ACL reconstruction sometimes requires repeat reconstruction. For further detailed information on repeat reconstruction, complications and the rehabilitation process can be found in the patient information booklet:
Patient Information and Rehabilitation Guidelines following Revision ACL reconstruction.pdf
Symptoms include pain, swelling and the knee giving way.
Surgery can involve either microfracture, autologous chondrocyte implantation (ACI) or Biopoly surgery.
Microfracture surgery can be performed to repair the defect by drilling multiple small holes in the bone. This causes bleeding and a formation of a blood clot. The clot encourages the formation of repair cartilage that fills the gap. Although it is not exactly like the articular cartilage it stops the bone rubbing on bone and helps reduce symptoms experienced.
Further detailed information on microfracture surgery, the complications and rehabilitation process can be found in the patient information booklet:
Patient Information and Rehabilitation Guidelines Following Microfracture Surgery.pdf
ACI involves the first operation to obtain cartilage from the patient’s knee (healthy part) and then grown in the lab to produce more cartilage cells. These cells are then implanted in the defected area as a second operation.
Further detailed information on ACI surgery can be found in the patient information booklet:
Patient Information and Rehabilitation Guidelines Following ACI Surgery.pdf
Biopoly surgery involves implanting a device, which uses an advanced biomaterial to resurface the defect in your knee joint.
Further detailed information on Biopoly surgery, the complications and rehabilitation process can be found in the patient information booklet:
The pain may increase when doing activities which repeatedly bend the knee, for example going up and down stairs, squatting, jumping and running. Prolonged sitting may also aggravate your pain.
Treatment involves an individually tailored physiotherapy programme.
Further information on anterior knee pain can be found in the patient information booklet:
Mr McNicholas has been using ECSWT for over 20 years, originally using the equipment that was used by Urology Surgeons for bursting kidney stones, with its settings at a lower energy level. Since 2012 Mr McNicholas has been using the Swiss Dolorcast® method, which uses a hand held probe to deliver radial shockwaves, and is specifically designed for treating musculoskeletal conditions. This tried and tested method has been used in over 100 million patients worldwide.
ECSWT is suitable for most patients who have chronically painful conditions for a minimum of 9-12 months despite appropriate treatment (physiotherapy, exercises or insoles for example) but in some circumstances may be used earlier, Mr McNicholas will discuss this with you at the appropriate time for your individual circumstances.
Download Patient information on Extracorporeal Shock Wave Therapy (ECSWT).pdf
Trauma
It is held in position by a number of ligaments, the most important is a ligament that runs from the inside edge of your kneecap to your thighbone. It is called the medial patella-femoral ligament (MPFL).
The kneecap can be displaced either by a direct blow or twisting injury or in people who have very lax ligaments or a shallow groove. When the kneecap dislocated it usually tears the MPFL ligament.
Sometimes it can heal without surgery if treated early, however if the kneecap keeps on dislocating you will need MPFL reconstruction surgery.
Further detailed information on surgery including MPFL reconstruction, trochleoplasty and tibial tubercle transposition, the complications and the rehabilitation process can be found in the patient information booklet:
This is a big injury which normally occurs when playing sports or in a road traffic accident.
The knee is held in place by numerous ligaments. When a knee dislocated some of these ligaments will be ruptured.
You will experience extreme pain at the time of injury and the knee will be swollen. In the emergency setting your knee will be put back into place. Your knee will also be checked for nerve and blood vessel damage which can occur with this injury.
Surgery will be required to reconstruct the damaged ligaments. Further detailed information on multi-ligament reconstruction surgery, complications and rehabilitation process can be found in this patient information booklet:
Patient Information and Rehabilitation Guidelines Following Multiple Ligament Reconstruction.pdf
Patient leaflet on ruptured extensor mechanism surgery and rehabilitation to follow.
Extensor Mechanism Repair Protocol


Pain
The end of the bones, where a joint is formed, is covered with articular cartilage. This provides a smooth slippery surface that allows the joint to move smoothly.
The problem occurs when the bone underlying the articular cartilage is injured. The blood flow to the bone is damaged and this small area of bone can die.
Diagnosis is made via a consultation, examination of the knee, x rays and MRI scan. Treatment includes non-surgical management in the first instance. If this does not work surgery may be required.
Further detailed information on osteochondritis dissecans, management options, complications and rehabilitation process can be found in the patient information booklet:
Patient Information And Rehabilitation Guidelines For Osteochondritis Dissecans (OCD).pdf
It is characterised by soreness and swelling over a bump (tuberosity) near the top of the shin bone (tibia) known as the tibial tuberosity. This tibial tuberosity may also increase in size as the condition progresses, and can affect one or both lower limbs.
Treatment involves a physiotherapy programme.
Further detailed information on Osgood-Schlatter Disease and physiotherapy exercises can be found in the patient information booklet:
It is usually a gradual process, at first the knee may be stiff but as the cartilage wears away and bone rubs on bone you are likely to feel pain.
The diagnosis is made during a consultation and an examination of your knee. X-rays are also taken.
There is no cure for osteoarthritis but can be managed in various ways. Treatment is dependent on your age, the type and level of your arthritis. During your consultation, the options available to you will be discussed.
Management options include:
- Non-surgical treatment
- High tibial osteotomy surgery
- Unicompartmental knee surgery
- Personalised knee replacement surgery
The following patient information booklets provide further detailed information on the above management options.
Patient Information on Osteoarthritis of the Knee and Non-surgical Management.pdf
14b-Patient-Information-And-Rehabilitation-Guidelines-Following-High-Tibial-Osteotomy-Surgery final